Disinfectant Compatibility Testing
For Reusable Medical Device Manufacturers
Identifying Compatible Cleaners and Disinfectants
We offer an accurate and efficient test service for assessing whether or not a hospital grade cleaner/disinfectant is safe to use with a reusable medical device. This allows device manufacturers to analyze the condition of their device after a lifetime of reprocessing and make informed, accurate decisions about which cleaners and disinfectants can be recommended to the end user. We understand that a reusable device may be reprocessed hundreds to thousands of times throughout its lifetime, making compatibility testing an inefficient and lengthy process. We’re here to help.
Ensuring Patient & User Safety
Healthcare personnel perform reprocessing to remove any visible soil (cleaning) and to inactivate microorganisms (disinfection or sterilization) prior to using/reusing a device. If the devices’ materials become damaged as a result of reprocessing, the risk of harm to a human/patient increases for a number of reasons:
The effectiveness of cleaning is critical to reducing microorganisms on a device as research shows that organic soil left on a device interferes with a germicide’s antimicrobial activity. 2
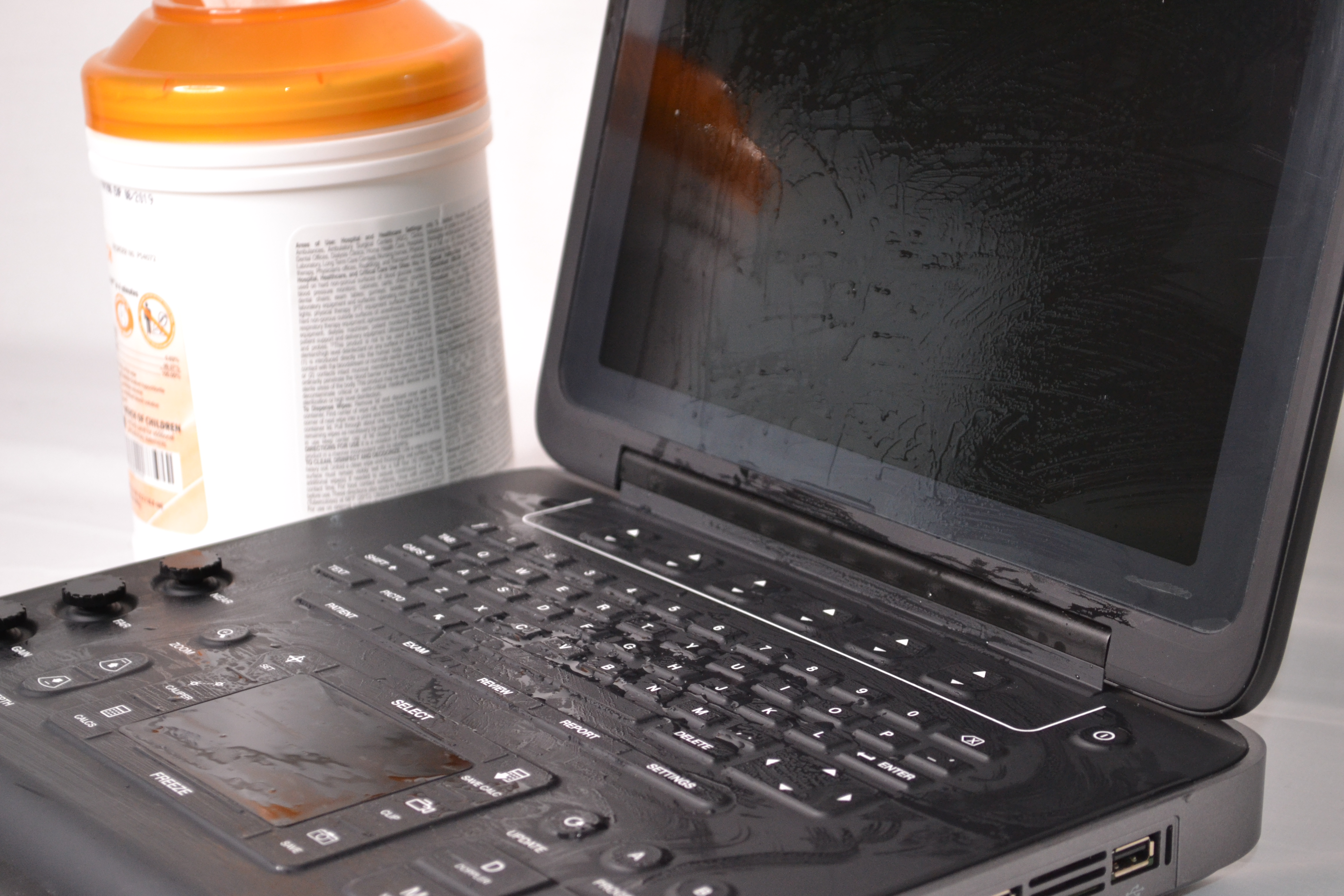
Cleaning will be less effective for device surfaces that become degraded, cracked, chipped, torn, etc. since these surfaces have increased roughness (more hiding places for microbes). Increased roughness has been shown to share a positive linear relationship with residual bacterial population and bacterial adhesion.3 This is believed to be caused by “an increase in surface area for adhesion and protection against shear forces at the wall.”4
References: 2. William A. Rutala, Ph.D., M.P.H. David J. Weber, M.D., M.P.H. and the Healthcare Infection Control Practices Advisory Committee (HICPAC) Guideline for Disinfection and Sterilization in Healthcare Facilities (2008)
3. Wang, H. , Feng, H. , Liang, W. , Luo, Y. and Malyarchuk, V. (2009), Effect of Surface Roughness on Retention and Removal of Escherichia coli O157:H7 on Surfaces of Selected Fruits. Journal of Food Science, 74: E8-E15. doi:10.1111/j.1750-3841.2008.00998.x
4. Characklis WG. 1981. Fouling biofilm development: a process analysis. Biotech Bioeng 23:1923–60.
Device housing materials that form a physical barrier between a devices’ internal electronics and users/patients are essential towards preventing electrical safety hazards. These materials are often plastics that are prone to environmental stress cracking if contacted by certain cleaners and disinfectants.1
References: 1. Hoffman JM, Ralston B, Chakravartula A, Reitman M. “ESC of Polycarbonate Exposed to Hospital Disinfectants,” Proceedings, ANTEC 2013, Society of Plastic Engineers, Cincinnati, OH, April 2013.
Materials that are damaged from cleaners and disinfectants may separate from a device, enter the sterile field, and increase the rate of adverse events. The biocompatibility of these materials may be unknown, especially if they are not expected to contact a patient. For instance, a recent search of the United States Food and Drug Administration (FDA) medical device recalls shows that the coating on a device used for surgical lighting “… may crack, posing the risk of particles falling into the surgical field during surgery that may result in patient infection.”5
References: 5. Medical Device Recall Z-1859-2019, www.fda.gov, April 2019.
We help reusable device manufacturers minimize these risks by replicating the standard operating procedures for reprocessing performed within the medical field. Given medical device test articles and the cleaning/disinfectant agent in question, we will repeatedly perform reprocessing according to the manufacturer’s instructions intended for the end user. Repeating this process for the number of expected device uses will allow manufacturers to identify and recommend cleaners and disinfectants that are safe to use.
Testing is Accurate and Efficient
Testing begins once a protocol is agreed upon with the reusable device manufacturer. Testing is conducted at our test lab in Arlington, WA.
To begin forming a protocol or to request more information, contact us.
Test Accuracy
We test devices just like the end user will reprocess them in the field. Although we will assess a device at any stage in it’s development (e.g. individual parts versus finished device) we suggest manufacturers test finished devices when validating a specific cleaner/disinfectant and device. We video record testing to ensure device degradation is not caused by damage unrelated to cleaning/disinfection (e.g. a device is dropped).
Test Efficiency
We employ multiple shifts throughout the day to ensure testing is completed efficiently. The length of one reprocessing cycle is usually dictated by the contact time indicated on the cleaner/disinfectant’s labeling and the size of the device being tested. Depending on these factors, we typically complete 200-600 reprocessing cycles per day.
Test Any Hospital Grade Cleaner/Disinfectant
Since we are an independent 3rd party we will test any commercially available hospital grade cleaner or disinfectant with your device. Often times cleaner or disinfectant manufactures will supply disinfectant wipes for testing at no charge!